For better or worse, the chances are you have strong opinions about police reform.
Even just the term “police reform” triggers many intense emotions, from both sides of the political spectrum, and doesn’t do any justice towards the actual meaning behind the idea.
Today, we answer the question – what does police reform mean?
We’ll cover the cause, effect, and specifics.
The Stigma Around Police Reform
Most people hear the term “defunding the police” and take it literally. To many, the term means “take away police funding, cut their salaries, remove police presence.” This is very far from the actual meaning of the term.
Police reform revolves around reallocating police funds and retraining officers, including their responses to drug offenses. While there are outliers with more radical views regarding police reform, they are just that – outliers. Financially, police reform calls for reducing the budget for weapons, non-community orientated programs, and changes in fines and fees associated with a drug arrest. However, the primary focus of funding has less to do with budget allocations and more to do with law enforcement’s response to drug use and mental health-related issues.
Currently, many emergency calls involving drugs or mental illness result in police taking aggressive action. Police officers are currently trained as soldiers, and as a result, they act like soldiers when they are called in. This type of mentality results in a lot of unnecessary violence and a negative stigma of the police in the public eye; For example, recently, a police officer who was responding to a disturbance call broke the arm of a 73-year-old woman with dementia while using force because she was not responsive to his commands. The police are supposed to make us feel safe, but many people are just afraid of them.
Under police reform laws, many drug-related and mental health emergencies would be handled by trained social workers, mental health professionals or simply allocate funds to train police officers in therapeutic counseling strategies of de-escalation. In all scenarios, officers would still be present in some capacity.
The Real-Life Results of Police Reform
Reallocating the police budget affects the entire community. It also narrows the scope of police work. Police are required to respond to virtually every emergency incident. This results in police being tasked with jobs that are outside of their expertise. For example, mental health calls require nuanced psychological training to have a positive outcome. The wide range of police work also contributes to elevated stress levels in officers due to the nature of their job and the effects of poor sleep and long working hours.
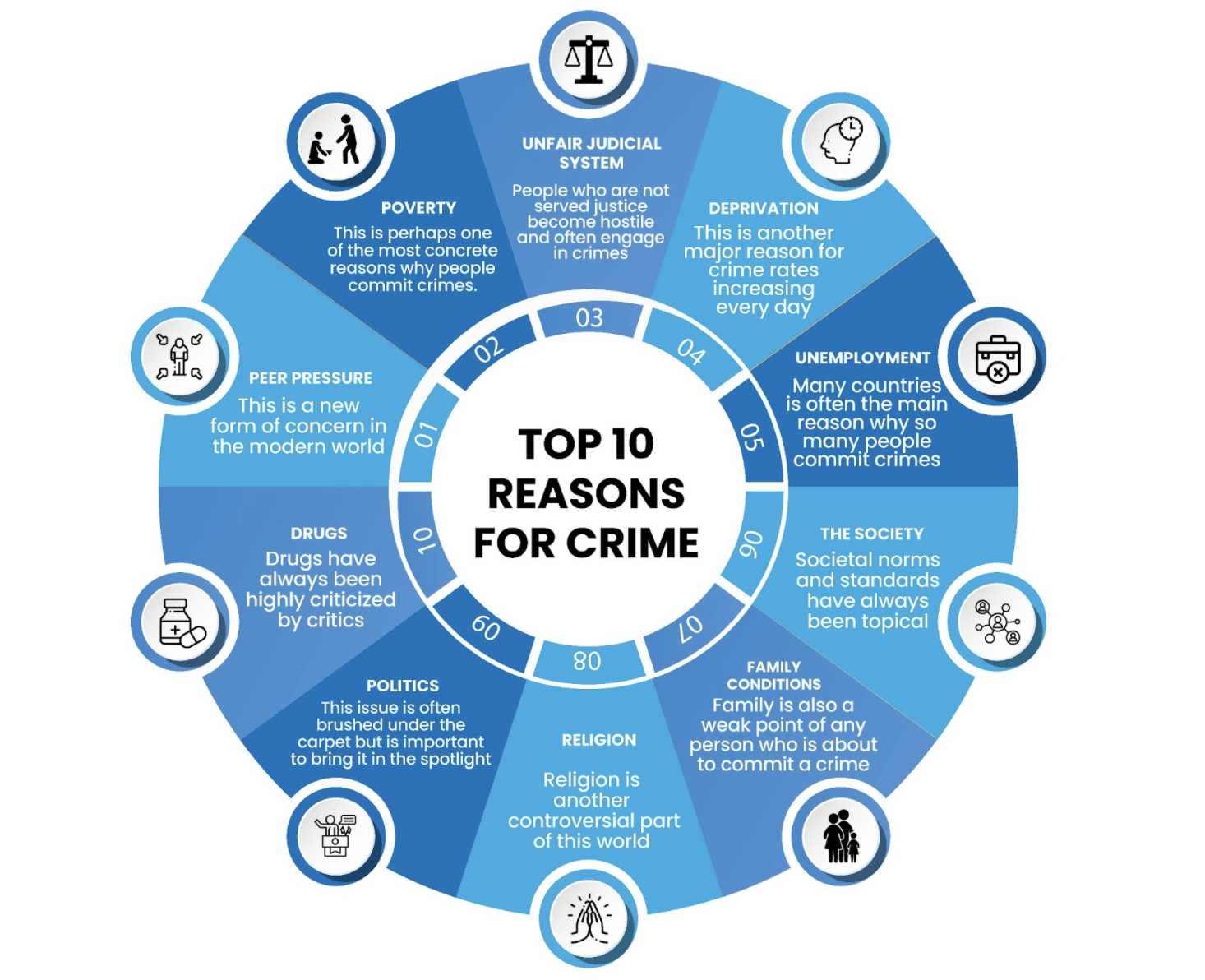
These are the most significant benefits of police reform:
- Improved Social Programs: Social programs encompass housing, education, and rehabilitation. Many social programs have extremely limited resources. This is especially true in impoverished neighborhoods. Youth that gets drawn into gang activity, drug experimenting, and other nefarious behavior often do so for lack of options. Community centers, sports, and stable housing reduce first-time offenses and provide long-lasting changes in any environment.
- Better Support for Mental Health: Individuals with mental health issues such as addiction, depression, PTSD, etc., often need help that most cops and jail environments cannot provide. Trained mental health professionals can only provide proper treatment. Commanding presences, like that exhibited by most law enforcement, only serve to intensify the harmful effects of mental instability.
- Reduced Violent Crime: As mentioned, cops often respond to non-violent, non-emergency situations. In police reform, officers would have more time and resources to focus on dangerous offenders and serious crimes.
Addiction as a Disease
Drug use is not a violent crime, but often authorities approach it as such. Addiction is a disorder of the brain, and drug use is a symptom of the disorder. Once you understand this, the idea of approaching the situation the same way you would a violent offender seems off base.
Historically, people viewed substance dependency as being caused by a lack of willpower or character. However, modern health professionals view addiction as a disease. Science shows genetics, environment, culture, and mental illness all play pivotal roles in developing an addiction. Children of substance-dependent parents are more likely to become addicted and/or suffer from behavioral issues.
Viewing addiction as a disease also allows for a more well-rounded treatment plan. This is due to the increasing focus on functional medicine. Functional medicine involves treating the patient’s entire body as a system- when one part fails, it affects the entire body. For example, depression and anxiety dampen the mood and disrupt logical thinking. A person suffering from these conditions may be unable to weigh the consequences of their addiction clearly. Additionally, people with the illnesses mentioned above may rely on substances to combat their depression, anxiety, and suicidal thinking.
Overcoming substance dependency requires time, therapy, and medical treatment. Without proper training, many officers may treat someone suffering from dependency the same as a violent offender. This can cause additional trauma and worsen the effects of mental illness and dependence on those affected.
It’s worth noting that police officers are not the only career that requires additional training regarding drug use. A societal change in thinking is necessary for long-lasting help and prevention to occur regarding drug dependency.
Many cities, such as Philadelphia, have taken to providing clean needles to people suffering from heroin dependency. Intravenous drug use is accountable for disease spread, severe infection, and other occurrences that put additional strain on city funds. Providing safe places and sanitized needles curb the risk of infection and violent crime. This is just one example of how changing societal views of addiction benefit both the community and the city budget.
Where Do We Go From Here?
The conversation surrounding police reform is still in its early stages. There have been several incarnations of police reform in the past that have worked to varying degrees.
An era of police reform occurred with the advent of digital cameras, phones, and internet crime. Police reform is a natural part of the institution; as society changes, so should the goal and practice of policing. The expectation of law enforcement moving forward is that officers will be limited in what calls they respond to en mass.

Police reform also limits their roles in mental health cases, non-violent disputes, and drug use. There is also a call for a higher level of accountability of police from their peers. To be clear, policing is as much a lifestyle as it is a career. It’s well known that officers, much like any life-defining career, form tight-knit groups that aren’t overly friendly to outsiders. This power level allows many police officers who commit crimes to receive reduced sentences, even when found guilty. The double standard afforded to officers during criminal proceedings only drives a wedge further between officers and the community they’ve chosen to protect.
While unit camaraderie and cohesion are essential to law enforcement, the cause and effect of these relationships can feel unfair. An officer can be loyal to their sworn code and still hold their fellow officers accountable.
Lastly, the combined factors of reduced violent activity, decriminalization of substances, and budget reallocation can increase the economic value of a neighborhood. This not only improves the economy and quality of life of its residents but also of communities nearby. As it stands, many non-violent offenders lose out on lifetime earnings, resources and gain social stigma for their drug use and arrests. A more lenient, support-based system allows persons with substance use issues to receive the treatment they need and reclaim their lives. To learn more about addiction recovery call the team at Anchored Tides Recovery at 866-600-7709.