In March 2020, life and the world as we know it changed, leading to many long-term side effects of the COVID-19 pandemic. These side effects are physical, including the potential for long-haul COVID to develop. Perhaps for some people, even more, damaging are the long-term effects on mental health during the COVID-19 outbreak.
Long-Term Effects of COVID Infection
Most people who have COVID get better in a few weeks. Some people, however, will experience long-term conditions related to the virus. The Centers for Disease Control and Prevention (CDC) describes this as post-COVID conditions.
Post-COVID conditions are a range of new, ongoing, or returning health problems you experience four or more weeks after initial COVID-19 infections. Even if you didn’t have symptoms or had very mild symptoms during an infection, you could still develop a post-COVID condition.
Long-term coronavirus disease symptoms can present differently and for varying lengths of time.
According to the CDC, some people experience different new symptoms lasting weeks or months after being infected, causing COVID-19. These possible long-term symptoms aren’t exclusive to people who were severely sick.
These symptoms can include:
- Problems breathing
- Shortness of breath
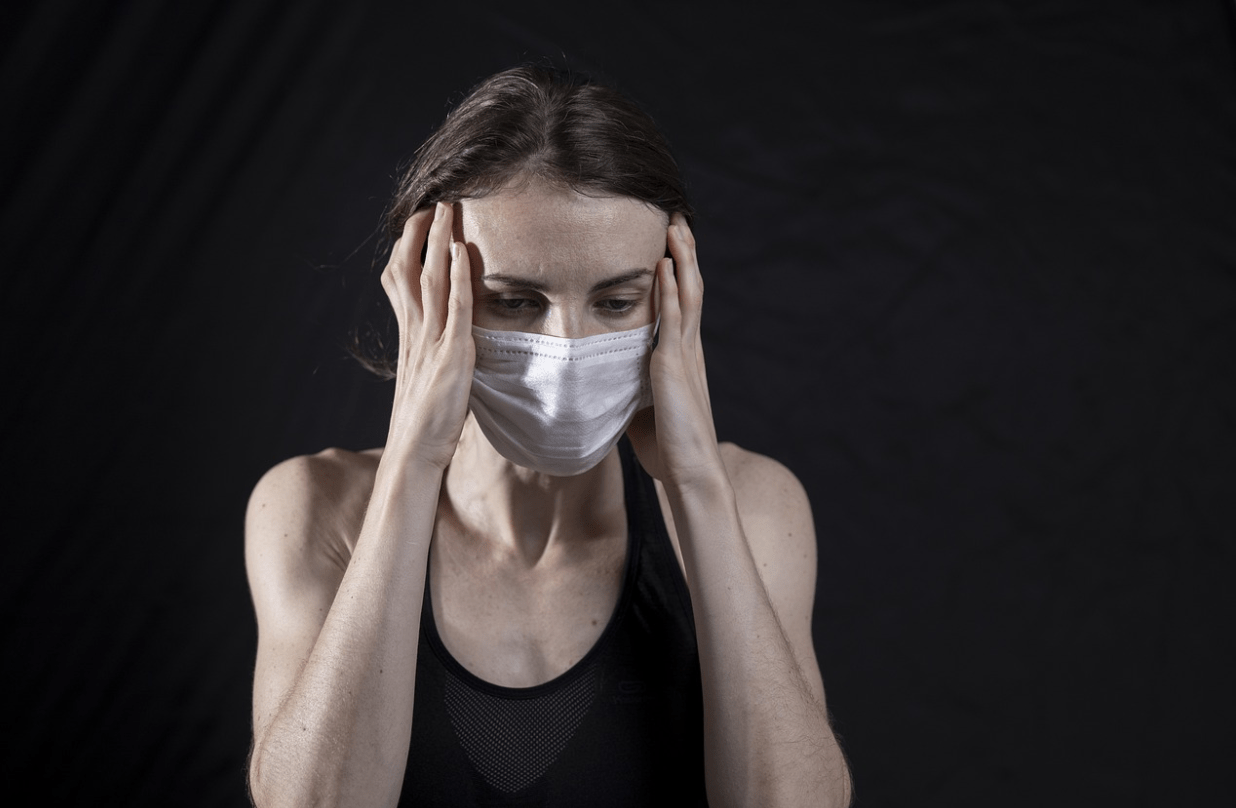
- Fatigue
- Brain fog
- Cough
- Headache
- Heart palpitations
- Pins-and-needles sensation
- Diarrhea
- Sleep disturbances
- Lightheadedness
- Changes in mood
- Joint pain
- Muscle pain
- General chest pain
- Changes in periods
- Alterations in smell or taste
While certain risk factors can make you more likely to have serious COVID-19, such as obesity or high blood pressure, there aren’t the same links to developing long-term problems. Doctors don’t know why some people deal with long-term effects while others don’t follow infection.
Multiorgan Effects
The CDC also has a category describing multiorgan effects of COVID and the development of autoimmune conditions. Autoimmune conditions occur when your immune system mistakenly attacks your healthy cells, leading to inflammation.
Symptoms in Teens and Children
Long-haul COVID is even less understood in teens and children than in adults, but complications are possible. Lingering COVID symptoms in younger people tend to include depression, fatigue, and shortness of breath.
Heart inflammation is another potential concern, especially in younger people.
Effects Following Severe Illness or Hospitalization
If you have COVID-19 and you’re hospitalized, you can experience severe fatigue and weakness as you recover. This is common for hospitalizations following any lung-related illness.
There’s also post-intensive care syndrome (PIICS). PICS is a health effect that starts in an intensive care unit (ICU). The symptoms remain even after you return home.
PICS can include problems with judgment and thinking, post-traumatic stress disorder, and severe weakness.
Neurological Complications
A fairly large portion of people who recover from COVID-19 disease goes on to report experiencing neurological complications like brain fog or confusion.
According to doctors, there are different possible treatments for these symptoms but not necessarily cures because we don’t yet fully understand the underlying causes.
For example, for neurological symptoms, available treatments may include medication, physical therapy, and psychotherapy for patients struggling with depression or anxiety or similar mental health concerns.
Cardiovascular Problems
There are currently several trials to understand more about the long-term effects of COVID on the heart. Around one-third of patients hospitalized with the virus have evidence in blood tests of heart injury.
Doctors think the heart damage comes from inflammation the viral infection triggers. That can lead to long-term heart problems, including heart attacks and abnormal heart rhythms.
Lung-Related Complications
We talked about this above, but various long-term lung complications can occur. Some people have problems breathing that don’t seem to get better. This problem may be due to blood clots causing scarring in the lungs. The scarring can then impact blood flow and reduce lung capacity.
Sense of Smell
One of the most commonly seen short- and long-term effects of the viral illness is loss of smell.
For this, often health care providers recommend olfactory training. Olfactory training requires you to smell different things in the morning and evening for several months. The goal is to stimulate your olfactory or smell nerves so they can regenerate.
Mental Health During COVID-19
The effects of the virus itself and infection aren’t the only long-term side effects of COVID-19. The mental health effects are proving to be pervasive and damaging. Even if you haven’t been directly affected by the virus itself or haven’t known anyone who’s gotten sick or died, you may still be struggling with mental health symptoms.
The pandemic has created stress and anxiety for many people, leading to emotional health issues and mental health disorders long-lasting without treatment.
Lockdowns led to isolation and financial worries. There are general health-related worries, so many people are experiencing. There are also fears that many people have specific to the virus, like the worry they or their loved ones will become seriously sick.
Based on history, health care providers say we know public health crises have a lasting impact on mental health.
Traumatic experiences like a pandemic are associated with higher post-traumatic stress disorder, depression, and substance use rates.
National surveys are starting to show the reality of how serious the mental health effects are. There is also a reduction in how many people seek treatment for substance use disorders and co-occurring mental illnesses. Those increased rates of substance use paired with less treatment initiation contribute to record high levels of overdose deaths.
Loss of Coping Mechanisms
Due to the pandemic, many people have lost a connection to their support networks and coping mechanisms. For example, maybe socializing was at one point a coping mechanism for many people, but now they’re worried about doing that.
Many people are still working from home, which reduces in-office social interaction, furthering the risks of isolation and mental health problems.
Maintaining a schedule can also be challenging if you are working from home or spending more time at home. Having a schedule is one form of a coping mechanism or protective factor against mental health symptoms and substance use disorders.
People continue to feel uncertain and out of control, worsening mental health symptoms.
What Can You Do?
Knowing that you aren’t alone if you’re personally experiencing long-term physical or mental symptoms stemming from COVID-19.
For physical symptoms, you should speak to your doctor. They may have recommendations to help you since so many people are going through them right now.
If you’re having symptoms of a new or worsening mental health or substance use disorder, call 866-600-7709 and talk to a team member of Anchored Tides Recovery. Again, many people are in the same situation as you, but you can take steps to get treatment.