The study of gateway drugs began nearly fifty years ago. While its hypothesis continues to face some controversy, the seriousness of drug abuse remains indisputable. If you currently suffer from addiction, things can improve from this point on. With the help of trained people who care, you can experience a better reality.
What Is A Gateway Drug?
A gateway drug is a substance that, when used, opens the door to the use of more harmful ones. They are addictive, relatively easy to access, and less potent than the more powerful and illicit substances for which they roll out the carpet.
The common usage of gateway substances by society puts them within the easy grasp of adolescents and young adults. They are made available by friends, schoolmates, siblings, and parents.
Growing up in a household in which at least one parent smokes cigarettes or drinks alcohol can automatically increase the chances that a youngster may eventually subscribe to the use of them. Although Mom or Dad may preach “do as I say, not as I do,” the visual example set by their behavior usually serves as the real teacher.
A Few Examples Of Gateway Drugs
A complete list of gateway drugs would likely face controversy, as many opposing views on the topic exist. Even so, substances that have stood the test of time as candidates usually fall under four general categories:
The Four Types Of Gateway Drugs
- Nicotine
- Alcohol
- Marijuana
- Prescription Opioids
Nicotine: The Gateway To The Hypothesis
When Dr. Denise Kandel coined the phrase “drug gateway” in the mid-seventies, she acted in a way that was contrary to others’ expectations. During that period, marijuana was the subject in the limelight. Her research project was supported and funded by those who hoped she would spotlight marijuana as a possible gateway drug.
Instead, she followed her inclination to place the focus on nicotine. Her efforts revealed that tobacco was the substance most likely to fit the bill as a gateway to others.
The initial stages of her research confirmed that youngsters were more prone, to begin with, to cigarettes, beer, and wine. After all, these were legal for adults and, therefore, more accessible to them.
Alcohol: The Culpable Companion
Both nicotine and alcohol have long been considered two partners in crime in the gateway drugs arena. The use of both has proven to be responsible for both short-term and long-term harmful consequences.
Research supports the notion that alcohol is the most widely used substance of these gateways. Whether or not it is the most likely to lead young people to polydrug use cannot change the well-known fact that excessive use of alcohol is detrimental to a high quality of life.
Is Marijuana A Gateway Drug?
There seems to be much controversy with classifying marijuana as a gateway drug. The inclination might be that it is not since most people who use it do not switch to using harder drugs.
However, the relaxing, sometimes euphoric, state that occurs while using marijuana reportedly diminishes over time with constant use. If it is resorted to as a means of escape from the stresses of everyday life, the quest to access more powerful, even illicit, drugs remains a possibility.
Prescription Opioids: Risky Business For Addictive Personalities
Opioids prescribed by doctors can effectively reduce mild to severe pain. They can also suppress coughs. Used properly, they have their place.
These drugs can also cause an intense high or euphoria, which often compels one to overuse them to continue re-experiencing that state. In turn, the user may be likely to seek out heroin, an illegal opioid.
Opioid abuse is out of hand. The United States is currently in the middle of an opioid epidemic. The effects of overdosing on them (most often unintentional) are catastrophic.
In 2022, scientific research continues. Much progress has emerged through molecular biology that shows evidence of gateway characteristics of how substances affect mice.
For example, such research has shown pretty conclusively that mice exposed to nicotine respond more readily to cocaine. Until more concrete evidence can parallel these findings with humans, it seems the hypothesis is yet to earn the status of qualifying as a theory.
Scientists have also exhaustively studied the use of alleged gateway drugs on a demographic level, looking for patterns and connections between the biological makeup of purported gateway drugs and their use.

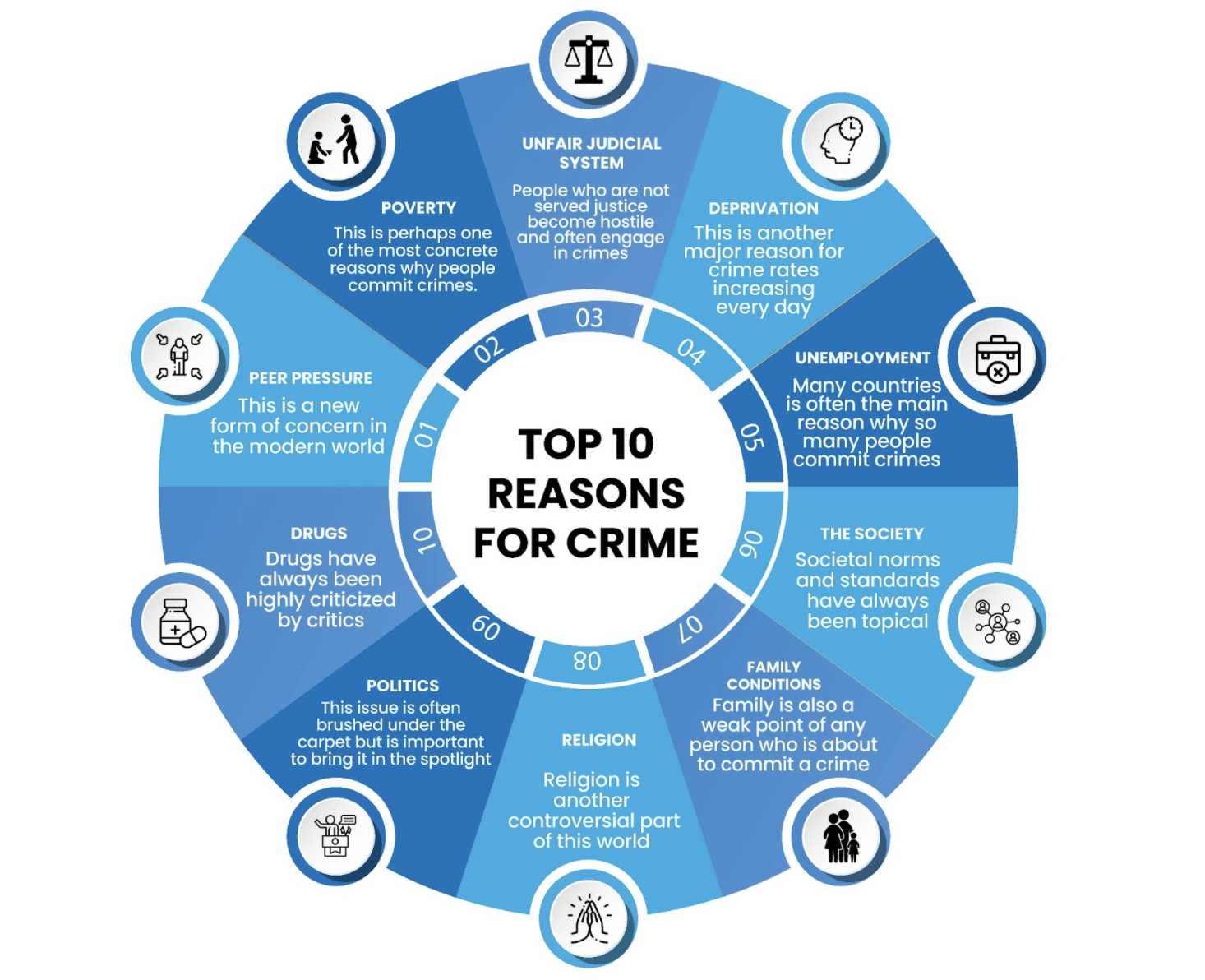
Addiction Goes Deeper Than The Drugs Themselves
Addiction goes beyond the scope of the attributes of drugs at a molecular level and demographics. Other factors contribute to the actions of an individual looking for relief, perhaps more than what can be fully understood.
However, some of these factors are not difficult to deny. People have individual characteristics, traits, personalities, backgrounds, and ways of handling life situations. These variables and more can contribute to the role a given substance plays in one’s life.
Science has a way to go. The attainment of conclusive evidence is still a goal. However, one significant fact that people can bank on is this: There is help available to people experiencing addiction challenges.
Women In Need Of Treatment For Addiction
In starting treatment, women often face certain obstacles that need to be acknowledged rather than avoided. The tendency to evade enlisting the help of others is all too common. Remember that, for every challenge, there is a solution.
For example, the stigma that often accompanies substance abuse is somewhat common among women. Also, the fear of losing child custody is a concern shared by mothers. Women with children facing addiction issues may face other obstacles, too. There may be countless excuses that an individual might see as valid reasons to delay seeking treatment.
The truth is that there is no legitimate reason to prolong the shackles of addiction when there are trained professionals who have effectively seen others through similar situations time and time again. Clinics specializing in helping women with addictions are fully aware that treatment is to be provided empathetically and in a way that addresses all the specific conditions of a woman’s life situation.
The Gateway To A Better Outlook On Life
If addiction is an issue in your life, acknowledging it and asking for help is a tremendous, notable stride toward recovery. Some people care and can, with your permission, help you to face each day with optimism.
Decide that, whatever it takes, you can get through any obstacles you might currently be facing. At the moment, things might seem a little murky. But the clouds always pass to make way for the sunshine. For you, the sky’s the limit.
If you, or someone you love, are struggling with addiction in Southern California, call 866-600-7709 and talk to an Anchored Tides Recovery team member today.