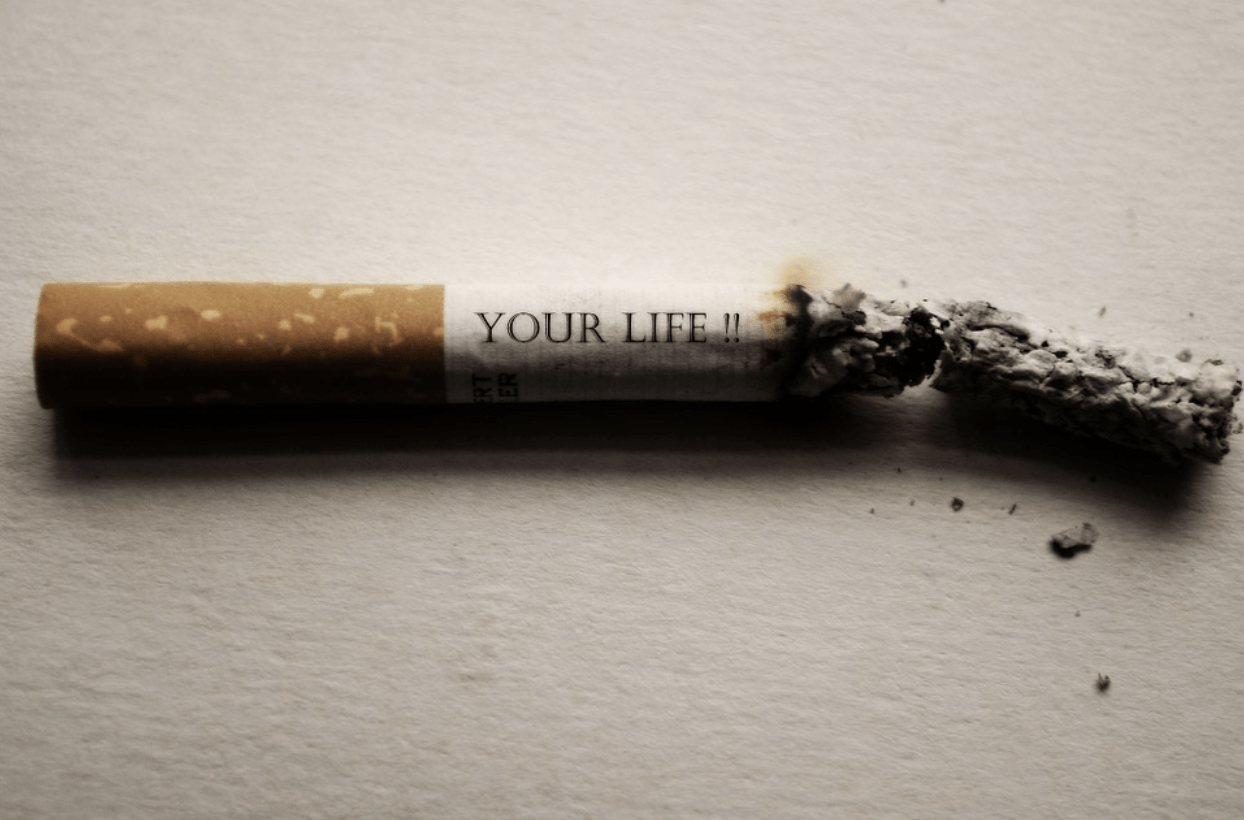
How to Navigate Addiction Recovery During the Holiday Season
The Christmas and New Year holiday season can be a time of joy but also stress, especially for those in addiction recovery. Social gatherings, family dynamics, and seasonal expectations may