In today’s fast-paced world, it’s common for individuals to seek relief from physical pain or emotional distress through various means. However, the combination of certain substances can pose significant risks to one’s health and well-being. One such dangerous combination is tramadol and alcohol. At Anchored Tides Recovery, we’re dedicated to providing you with the knowledge and support you need to make informed decisions about your health. In this comprehensive guide, we’ll delve deep into the intricacies of mixing tramadol and alcohol, exploring the potential dangers, physiological effects, and the importance of seeking professional help. If you or a loved one is struggling with tramadol or alcohol addiction, we urge you to take the first step toward recovery by contacting us today.
What Happens When Tramadol and Alcohol are Combined?
Understanding Respiratory Depression
- Serious Concern: Respiratory depression is a critical issue that arises when tramadol, a potent opioid pain reliever, and alcohol, a central nervous system depressant, are combined.
- Suppression of CNS: Both substances exert their effects by depressing the central nervous system (CNS), including the vital respiratory centers located in the brainstem.
- Compound Effects: When tramadol and alcohol are consumed together, their depressant effects synergize, leading to a pronounced suppression of respiratory function.
- Symptoms: This can manifest as shallow breathing, labored respiration, difficulty catching one’s breath, and in severe cases, complete respiratory arrest.
- Emergency Attention Needed: It’s crucial to recognize the signs of respiratory depression and seek immediate medical attention, as this condition can rapidly deteriorate into a life-threatening emergency if left untreated.
The Mechanisms of Central Nervous System Depression
- Brain Neurotransmitter Inhibition: Central nervous system depression occurs when neurotransmitter activity in the brain is inhibited, leading to a decrease in overall brain function and slowed communication between neurons.
- Enhancement of GABA: Both tramadol and alcohol enhance the activity of gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter. This results in a cascade of effects, including sedation, relaxation, and a reduction in anxiety levels.
- Synergistic Effects: When tramadol and alcohol are taken together, their effects on GABAergic neurotransmission synergistically potentiate the depressant effects on the central nervous system.
- Heightened Risks: This heightened depression of CNS activity increases the risk of cognitive impairment, including confusion, disorientation, and memory problems. Motor function may also be severely impaired, leading to difficulties with coordination and balance, while loss of consciousness becomes a significant concern.
The Potential for Addiction
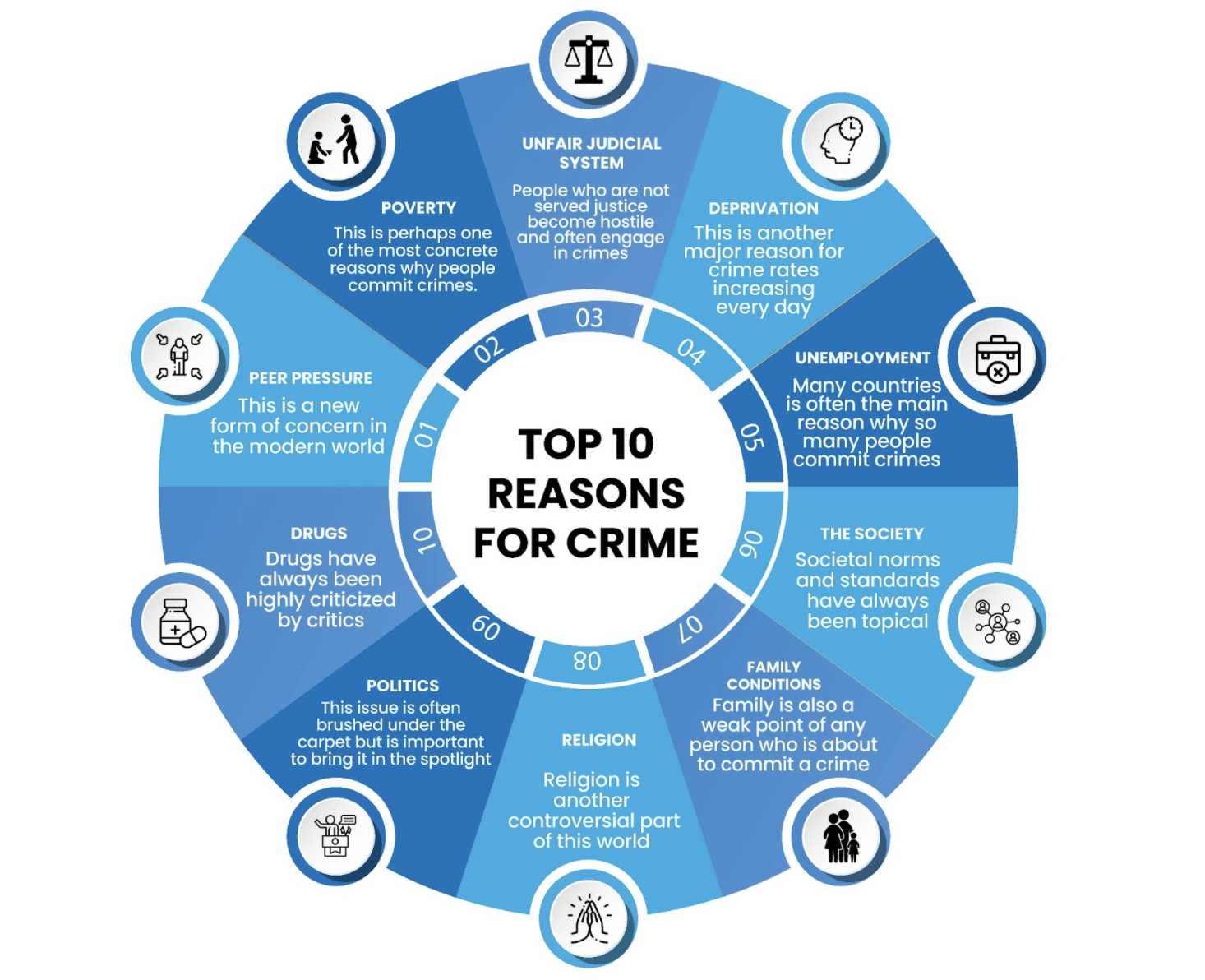
- Significant Concern: Addiction is a pervasive and complex issue associated with the chronic misuse of tramadol and alcohol.
- Brain Chemistry Alteration: Both tramadol and alcohol can induce significant alterations in brain chemistry, particularly within the brain’s reward circuitry. These changes can lead to the development of tolerance, wherein increasingly larger doses of the substances are required to achieve the desired effects, as well as physical and psychological dependence.
- Reward System Changes: Chronic use of tramadol and alcohol can hijack the brain’s natural reward system, causing individuals to experience intense cravings for the pleasurable effects produced by these substances.
- Compulsive Behavior: Over time, this can culminate in a pattern of compulsive drug-seeking behavior, wherein the individual prioritizes obtaining and using tramadol or alcohol above all other aspects of their life, despite experiencing negative consequences such as relationship problems, financial difficulties, and deteriorating physical health.
- Need for Professional Help: Given the complex interplay of biological, psychological, and social factors involved in addiction, seeking professional help from a qualified treatment provider is essential for addressing tramadol addiction or alcohol addiction effectively.
DON'T WAIT ANY LONGER...
Why Seeking Alcohol Addiction Treatment is Crucial
If you or someone you know is struggling with tramadol or alcohol addiction, seeking professional help is paramount to reclaiming your life and achieving lasting sobriety. At Anchored Tides Recovery, we understand the unique challenges faced by women battling addiction, and we’re here to provide you with the support and guidance you need to heal. Our comprehensive women’s rehab programs in Huntington Beach, CA, are designed to address the specific needs of women, offering a safe and nurturing environment for recovery. Through evidence-based treatments, individual therapy, group counseling, and holistic modalities, we empower women to overcome addiction and embrace a healthier, more fulfilling life.