What Makes Women’s Addiction Treatment Unique?
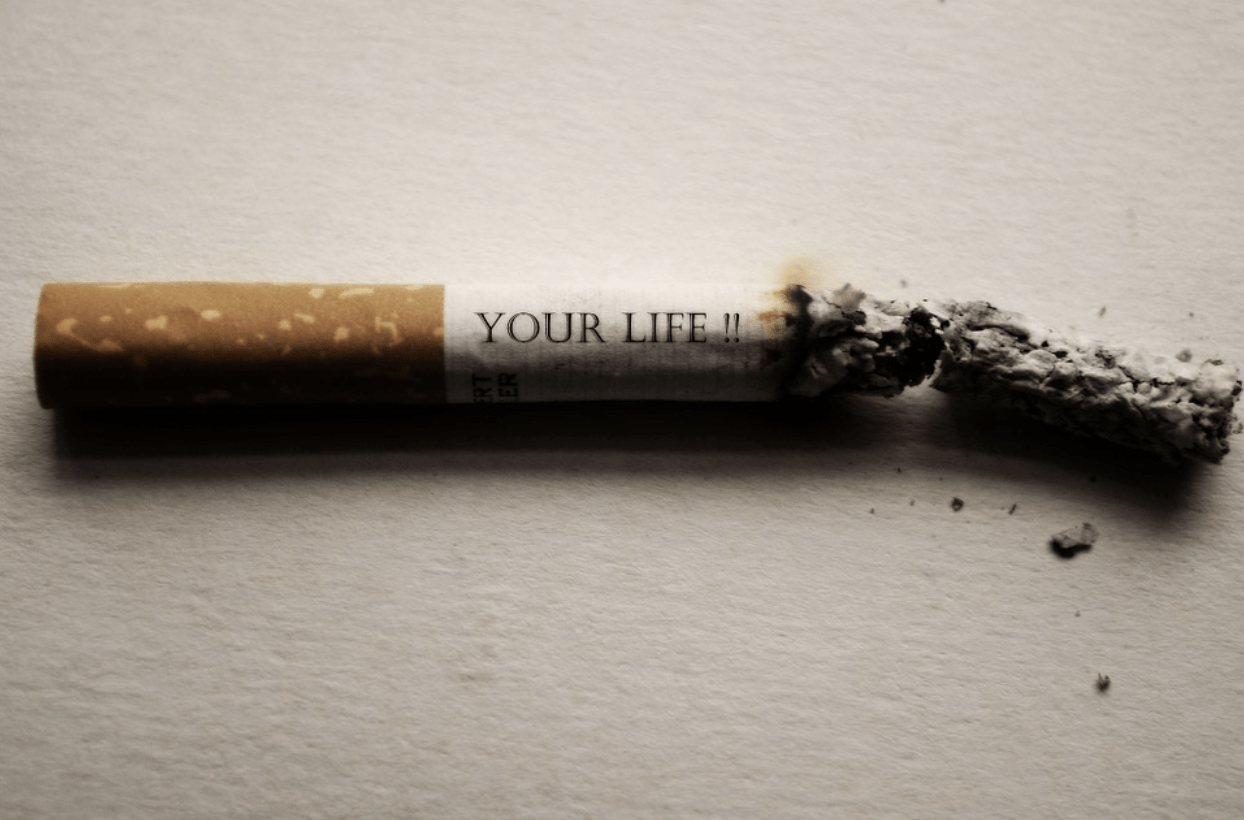
Addiction doesn’t discriminate, but the journey to recovery often looks different for women. Women face unique challenges when it comes to substance use, including societal pressures, family responsibilities, and higher rates of trauma. These factors necessitate treatment approaches tailored to women’s specific needs. We explore what makes women’s addiction treatment unique, from gender-specific rehab programs and trauma-informed care to holistic therapies and specialized support for mental health and dual diagnoses.
The Importance of Gender-Specific Rehab for Women
Women’s experiences with addiction are distinct from men’s, often influenced by emotional, psychological, and social factors. Gender-specific rehab programs recognize these differences and create safe, supportive environments where women can openly discuss their struggles without judgment. These programs focus on issues like body image, self-esteem, motherhood, and relationship dynamics, which are often central to women’s addiction journeys. By addressing these gender-specific concerns, women’s rehab programs foster stronger connections and more effective healing.

Unique Challenges in Female Substance Abuse Recovery
Women face unique barriers in their recovery journey, including societal stigma and family obligations. Many women are primary caregivers, which can complicate their ability to seek treatment. Additionally, women are more likely to have experienced trauma, such as domestic violence or sexual abuse, which can contribute to substance use. Emotional factors like guilt and shame, along with co-occurring disorders such as anxiety and depression, further complicate the recovery process. Understanding these challenges is key to providing effective support.
What is Trauma-Informed Care?
Trauma-informed care is a treatment approach that recognizes the widespread impact of trauma on an individual’s life and recovery. It prioritizes creating a safe and supportive environment where patients feel respected and empowered. In women’s rehab programs, trauma-informed care is essential due to the high prevalence of trauma among women struggling with addiction. This approach incorporates practices that avoid re-traumatization and promote healing, such as empathetic communication, individualized treatment plans, and holistic therapies.
Trauma-informed Related Articles
Holistic Approaches in Women’s Addiction Treatment
Holistic addiction treatment goes beyond addressing substance use; it focuses on healing the whole person—mind, body, and spirit. For women, holistic methods like yoga, mindfulness, art therapy, and nutrition play a crucial role in recovery. These therapies help women manage stress, process emotions, and build resilience. By integrating holistic practices with traditional therapies, women’s rehab programs offer comprehensive care that supports lasting recovery.
Women’s Intensive Outpatient Programs (IOP)
Women’s Intensive Outpatient Programs (IOPs) provide flexible treatment options that allow women to receive comprehensive care while maintaining their daily responsibilities. These programs are ideal for women who need structured support but cannot commit to residential treatment. IOPs offer group therapy, individual counseling, and holistic treatments, fostering a sense of community and ongoing support. This balance of treatment and real-life integration is particularly beneficial for women managing family, work, and recovery.
Addressing Substance Use Disorder, Mental Health, and Dual Diagnosis
Substance use disorder often coexists with mental health conditions, a situation known as dual diagnosis. For women, common co-occurring disorders include anxiety, depression, obsessive-compulsive disorder (OCD), and postpartum depression. These conditions can exacerbate substance use and complicate recovery. Integrated treatment that addresses both addiction and mental health is essential for successful outcomes. Women’s addiction programs focus on understanding these interconnected issues and providing comprehensive care that supports both mental health and sobriety.
Anchored Tides Recovery holds a very special place in my heart. I have seen their work first hand with their clients and they do amazing things. To find a Women's Facility can be difficult but to find one that actually cares for their clients, goes above and beyond to help them and genuinely has the client's best interest in mind is sometimes impossible. I would recommend any female that is struggling with addiction in someway shape or form reach out to Anchored Tides. They do amazing work with trauma, mental health and substance use disorders.

Specialized Care for Veterans and Military Women
Female veterans face unique challenges in addiction recovery, including the effects of military-related trauma and the difficulties of reintegration into civilian life. Specialized programs, like those offered at Anchored Tides Recovery, address these specific needs. These programs provide targeted support for PTSD, trauma, and mental health issues common among female veterans, ensuring a safe and understanding environment for recovery.
Why Choose a Women’s Recovery Center?
Choosing a women’s recovery center offers numerous benefits, from specialized treatment plans to a supportive, understanding community. Women’s recovery centers focus on creating safe spaces where women can share their experiences and support one another. The sense of sisterhood and shared understanding fosters deeper healing and connection. For more information on tailored programs, visit our Women’s Recovery Center.
Taking the First Step: Your Journey to Recovery Starts Here
Women’s addiction treatment is unique because it addresses the specific emotional, psychological, and social factors that affect women in recovery. From gender-specific rehab and trauma-informed care to holistic therapies and specialized mental health support, these tailored approaches provide the tools needed for lasting recovery. Ready to start your journey? Contact us today to learn more about our women’s addiction treatment programs and find the support you deserve.
FAQ: Helping a Loved One Through Women’s Addiction Recovery
Look for signs like changes in behavior, withdrawal from family and friends, neglecting responsibilities, and physical health issues. If you notice these, it might be time to have a compassionate conversation about seeking help.
Use empathetic language. Let them know you care and are concerned about their well-being. Avoid judgment and focus on their health and future. For example, “I’m here for you, and I want to help you find the support you deserve.”
Yes, women’s addiction treatments address unique challenges like trauma, family responsibilities, and co-occurring disorders. Programs often include gender-specific counseling, holistic therapies, and trauma-informed care.
Stay involved in their recovery process. Attend family therapy sessions if possible, offer emotional support, and be patient. Encourage healthy habits and celebrate their progress.
If they refuse treatment, continue offering support without enabling harmful behaviors. Consider speaking to a professional about intervention options and setting healthy boundaries.
You can find specialized programs through resources like our [Women’s Recovery Center](https://anchoredtidesrecovery.com/womens-addiction-treatment-center/womens-drug-rehab/), which offers tailored support for women in recovery.

















 In a world where the prevalence of depression continues to rise, finding effective and alternative treatments is of paramount importance. One such alternative that has been gaining attention is heated yoga. In a groundbreaking randomized controlled clinical trial conducted at Massachusetts General Hospital, researchers discovered that participants who engaged in heated yoga sessions experienced significant reductions in depressive symptoms compared to a control group. This exciting development suggests that heated yoga could be a promising addition to the arsenal of treatments for individuals suffering from moderate-to-severe depression.
In a world where the prevalence of depression continues to rise, finding effective and alternative treatments is of paramount importance. One such alternative that has been gaining attention is heated yoga. In a groundbreaking randomized controlled clinical trial conducted at Massachusetts General Hospital, researchers discovered that participants who engaged in heated yoga sessions experienced significant reductions in depressive symptoms compared to a control group. This exciting development suggests that heated yoga could be a promising addition to the arsenal of treatments for individuals suffering from moderate-to-severe depression.