Understanding Suicide and Its Warning Signs
Suicidal thoughts don’t always look the way we expect. Sometimes, they’re loud—like someone openly expressing their pain. Other times, they’re quiet—like someone slowly withdrawing, losing interest in life, or feeling like a burden to those around them.
If you’re worried about a loved one, you’re not alone. Many families, friends, and partners struggle with how to recognize and respond to suicidal ideation. We will help you identify suicidal warning signs, suicide risk factors, and ways to offer support before a crisis happens.
At Anchored Tides Recovery, we understand the deep emotional pain that can lead someone to feel hopeless. We also believe in the power of connection, healing, and recovery.
What Is Suicidal Ideation?
Suicidal ideation refers to thoughts about ending one’s life, whether fleeting or persistent. There are two main types:
Passive Suicidal Ideation
A person has thoughts of not wanting to exist but no specific plans to act on them. Examples include:
- “I wish I could just disappear.”
- “I wouldn’t care if I didn’t wake up tomorrow.”
Active Suicidal Ideation
A person is not only thinking about suicide but has a plan to act on it. They may:
- Express thoughts of self-harm
- Gather means (such as pills or weapons)
- Say goodbyes or settle unfinished business

How Common Are Suicidal Thoughts?
Not everyone who struggles with suicidal thoughts shows obvious signs, but certain behaviors, emotions, and verbal cues may indicate a person is at risk.
Behavioral Warning Signs
- Social withdrawal – Avoiding family, friends, and social events
- Increased substance use – Drugs or alcohol may be used to numb emotional pain
- Sudden calmness after distress – May indicate a decision to act on suicidal thoughts
- Reckless or self-destructive behavior – Engaging in dangerous activities without concern for consequences
- Giving away possessions – Especially meaningful or sentimental items
Emotional Warning Signs
- Feeling trapped or hopeless – Expressing that “nothing will ever get better”
- Extreme guilt or shame – Feeling like a burden to others
- Severe mood swings – Going from deep despair to sudden relief (which may signal an intent to act)
- Increased anxiety or agitation – Restlessness, irritability, or difficulty concentrating
Verbal Cues to Look Out For
- “I just can’t do this anymore.”
- “Everyone would be better off without me.”
- “I don’t see the point in anything.”
- “I’m just tired of fighting.”
If you hear someone express thoughts of suicide, take it seriously. Don’t assume it’s just a passing thought.
Suicide Risk Factors
Certain factors can increase the likelihood of suicidal ideation. These don’t necessarily mean someone will attempt suicide, but they are red flags that shouldn’t be ignored.
- Mental health conditions – Depression, anxiety, PTSD, bipolar disorder
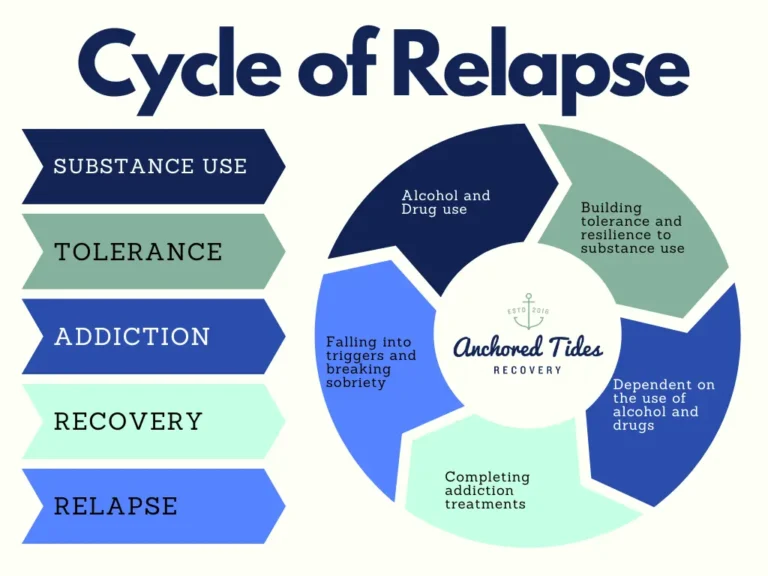
- Substance abuse – Drug and alcohol use can increase impulsivity and worsen depression
- History of trauma or abuse – Childhood trauma, domestic violence, or sexual assault
- Chronic illness or disability – Ongoing pain or health struggles
- Recent major loss – Death of a loved one, job loss, or a breakup
- Previous suicide attempts – History of self-harm or suicide attempts increases future risk
If someone in your life has multiple risk factors, stay connected. Isolation makes these risks even greater.
How to Help Someone Struggling with Suicidal Thoughts
- Start the Conversation
Many people fear saying the wrong thing, but silence is far more dangerous. Ask directly and with compassion:- “I’ve noticed you’ve been struggling—are you thinking about hurting yourself?”
- “You’re not alone. Can we talk about what’s going on?”
- Listen Without Judgment
- Let them speak freely without minimizing their feelings.
- Avoid saying things like “Just think positive” or “You have so much to live for”. Instead, say:
- “I hear you, and I’m here for you.”
- “I want to help. Let’s find support together.”
- Remove Access to Dangerous Items
If your loved one has mentioned a specific plan, take action immediately:- Remove medications, firearms, or other means of self-harm.
- Stay with them or have someone they trust keep them safe.
- Encourage Professional Help
Therapy, crisis hotlines, and medical support can save lives. If they are resistant, offer to:- Call a crisis helpline with them
- Help them find a therapist or treatment program
- Stay by their side as they seek support
At Anchored Tides Recovery, we specialize in treating co-occurring mental health and substance use disorders because healing requires addressing both.

Suicide Awareness Month: September 2025
Every year, September is Suicide Prevention Awareness Month, a time dedicated to breaking the stigma and spreading hope.
Ways to Get Involved:
✅ Share resources on social media
✅ Participate in local awareness walks or events
✅ Support someone who is struggling by checking in
Raising Awareness Slogan:
“You are not alone. Hope is real. Help is available.”
Even the smallest act of support can save a life.
You Matter
If you or someone you know is struggling with suicidal thoughts, please know:
- “Your life matters, even when it doesn’t feel like it.”
- “You are not a burden. You are loved.”
- “This pain won’t last forever—there is help.”
You are not alone. If you need immediate help, please call the Suicide & Crisis Lifeline at 988.
At Anchored Tides Recovery, we are here to support healing and recovery. If you or a loved one is struggling, reach out today. 💛
If this article helped you, share it. Together, we can break the silence and offer hope.